It is a well-researched and broadly understood phenomenon that information technology (IT) has driven economic growth in recent decades and, especially with the onset of artificial intelligence, it will likely do so into the future. Many companies have directly experienced IT’s effects on how they conduct business. For example, IT has transformed how managers coordinate, communicate, and guide production to improve output and enhance product quality. And some companies owe their existence to advances in IT.
Given the importance of IT, and the competitive pressures that advances bring to the market, you might think that a company would have an unlimited appetite for IT investment. However, capital expenditures (capex) are expensive, and the future is unknown. While large IT investments can positively impact a firm’s growth, a failed investment can have equally large negative effects. Market uncertainty, it turns out, is key to firms’ decision-making. However, research has offered limited insight into how market fluctuations affect firms’ IT investment decisions.

This paper addresses that gap by employing an empirical approach that captures the relationship between market events and long-term IT capex budgeting. For example, if firms do respond to changes in market circumstances, it is not clear whether IT capex adjustments would simply mirror other short-run spending decisions or diverge from other business actions. These decisions can be quantified. In other words, how market shocks influence firms’ IT adoption decisions is an empirical question. Answering this question helps explain the uneven spread of IT across and within industries.
The authors focus on health IT, specifically of US hospitals. The US hospital industry captures over $1 trillion (about 30%) of medical spending annually––the largest share of spending among the provider types. The health IT adoption in decision is ideally suited for the authors’ investigation because hospitals must commit to substantial upfront investment while accepting potentially large adjustment costs: in economics, these are expenses incurred when economic agents (like firms or individuals) change their decisions or actions, such as adjusting production levels, hiring or firing workers, or investing in new capital and sunk costs: an expense or investment that has already been made and cannot be recovered, regardless of future decisions tied to health IT procurement. Hospitals also face uncertain payoffs and are regularly exposed to business cycle fluctuations as well as industry-targeted policy and regulatory interventions.
The authors study industry-specific microdata that captures nearly all hospitals, including granular information on the timing and type of IT investments made over time, as well as negative shocks: an unexpected event that has a detrimental impact on the economy, potentially leading to decreased output, increased unemployment, and higher prices, for example (e.g., the Great Recession of 2008-09) and positive shocks: an unexpected event that leads to a beneficial increase in economic activity, such as increased production, lower prices, or higher employment, often stemming from either increased demand or supply (e.g., the 2014 Affordable Care Act Medicaid expansions) to find the following:
Hospitals’ IT investment decisions are sharply influenced by harmful and helpful market shocks
in a symmetrical manner; that is, economic downturns restrain hospitals’ investments while hospitals exposed to a Medicaid expansion purchase more health IT.
The effects of both shocks are dynamic and become larger with time. Three years after the financial crisis, hospitals operating in the most severely impacted areas decrease their IT capital investments by 10% to 15%. Similarly, hospitals affected by the 2014 Medicaid expansions adopt nearly 10% more technology solutions in comparison to hospitals in non-expansion states by 2017.
- Hospitals’ adjustments include clinical service-line management, laboratory management, and multiple administrative functions (e.g., back-office management, financials, information systems, and utilization review).
- The relative effect sizes typically range between 5% to 15% for a given technology purpose; however, some changes are as large as 30% to 67% over baseline levels. These behavior changes are present among for-profit as well as not-for-profit hospitals and are statistically indistinguishable between the two.
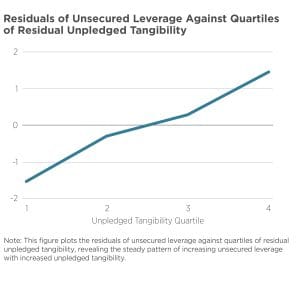
- The impacts on hospitals’ decision-making are not fully explained by pure income shocks: one-time, unexpected changes in how much money an individual or firm earns or has . Standalone and financially weaker hospitals are not more responsive to either shock; rather, their responses are more muted at times. And hospitals with relatively greater exposure to the size of the Medicaid expansions do not engage in greater health IT capital investments compared to other hospitals in affected states.
- Finally, these observed changes in IT investment do not apply to more variable hospital expenditures, like hiring and marketing. This new finding emphasizes that hospitals prioritize the IT capital investment margin differently when facing changes in financial and market circumstances.
One policy implication of this novel research: Building on work that calculates the implied “savings” for states refusing to expand Medicaid through the ACA, the authors reveal a previously overlooked, indirect consequence of state policymakers’ decisions; namely, they are restraining technological investment within their own hospital industry. Such decisions further challenge ongoing attempts by US healthcare firms to leverage IT advancements to improve performance.