More than half of Americans over age 65 and 13% of all Americans are covered by more than one source of health insurance. This overlapping coverage creates “administrative fragmentation,” or the lack of standardization in billing and administrative processes across payers. The resulting complexity can lead to costly inefficiencies and frustrating delays or denials for patients and providers. But how much do these inefficiencies actually matter?
In this paper, the authors study a major Medicare reform that consolidated administrative contracts for hospital and outpatient claims within jurisdictions, eliminating the need for multiple parties to handle processing different parts of the same patient’s care. Importantly, while the reform simplified billing processes, it left other factors—such as payment rates and benefits—unchanged, allowing the researchers to isolate the effects of administrative fragmentation.

Using Medicare administrative data from 2007-2017 and leveraging the staggered rollout of the reform across jurisdictions, the authors compare hospitals with varying baseline levels of administrative fragmentation to estimate causal effects. They find the following:
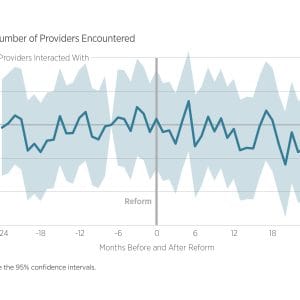
- Administrative fragmentation fell sharply. The share of patients who encountered multiple administrative entities during and after hospital stays declined by more than 35 percentage points following the reform.
- Improvements in administrative efficiency were modest. The reform led to a small (2.3%) reduction in denial rates for physician services delivered after hospital discharge, but had no measurable effect on the time it took to process claims.
- Hospital administrative costs and technology adoption remained unchanged. There was no evidence that the reform reduced hospital-reported administrative costs or increased the adoption of billing software and other administrative technologies by hospitals or outpatient providers.
- There was no effect on patient care or outcomes. The authors find precise null effects on downstream utilization, total Medicare spending, provider access, and 30-day hospital readmission rates.
These findings suggest that streamlining billing alone is unlikely to reduce administrative costs or meaningfully affect patient care or outcomes. The authors caution that simply routing all claims through a single administrative entity does not, on its own, improve efficiency or care delivery. It is possible that broader efforts to harmonize other aspects of payer fragmentation, such as inconsistencies in payment rates, coverage rules, and eligibility criteria, may be generate more substantial improvements.